Snoring Treatment
The decision to approach surgery in patients with snoring and sleep apnea depends on many factors. Patients’ complaints can vary from a simple snoring to a severe clinical picture accompanied by an increase in lung blood pressure, the area of blockage is not limited to a single region, but several anatomical regions may participate in the event to different degrees.
The general condition of the patients and other medical problems such as high blood pressure, diabetes, heart disease also play an important role in making the surgical decision.
The main points that suggest the decision to operate in this disease group, where a wide variety of surgical techniques can be used, are;
In sleep analysis (Polysomnography), the RDI (Respiratory disturbance index) is above 20,
Detection of blood Oxygen saturation below 90% by polysomnography,
How complaints such as drowsiness throughout the day affect daily life,
Having a pronounced heart rhythm disorder,
Detection of obvious anatomical problems that will explain the complaints during the examination of the patient,
The fact that he did not benefit from other conservative treatment methods,
Inability to adapt to CPAP treatment,
There is no medical problem that will prevent the operation from being performed.
A. OPERATIONS FOR SOFT PALATE
The aim of this type of surgery is to increase the volume of the air passage behind the small tongue and soft palate and to reduce the tendency of tissue collapse. Although it is the most common surgical area, the problem is limited to only this area in only a quarter of patients.
About half of the patients have problems with the tongue root or nose area along with the palate. As a result, it can be said that 75% of patients have more or less soft palate and small language problems.
The type of surgery to be performed for the soft palate varies depending on the severity of the problem and the cause of airway obstruction. In addition to sleep analysis, the small tongue (Uvula), soft palate, posterior side walls of the throat (lateral pharyngeal bands) and tonsils should be carefully evaluated when deciding on the intervention to be performed.
In general, there are five types of surgical approaches:
- Palate radiofrequency applications:
It is based on the principle of creating heat damage that heals with contraction and hardening of the tissues and palate muscles under the mucous membrane with the energy supplied to the soft palate tissue by radiofrequ November. As a result, there is a decrease in the tendency of the soft palate to tremble and collapse with the vacuum created by the air flow. The procedure can be performed under local anesthesia under office conditions (figure 1).
It is preferred in patients where there is a limited amount of thickening, degeneration and sagging of the soft palate, usually a snoring complaint and without significant apnea, or in patients with mild soft palate problems and the main pathology causing apnea is in other areas. Better results are obtained in patients with a body mass index (Body mass index) below 25, and results get worse and worse at values above 25.
2.Soft palate implant application (Pillar Implant):
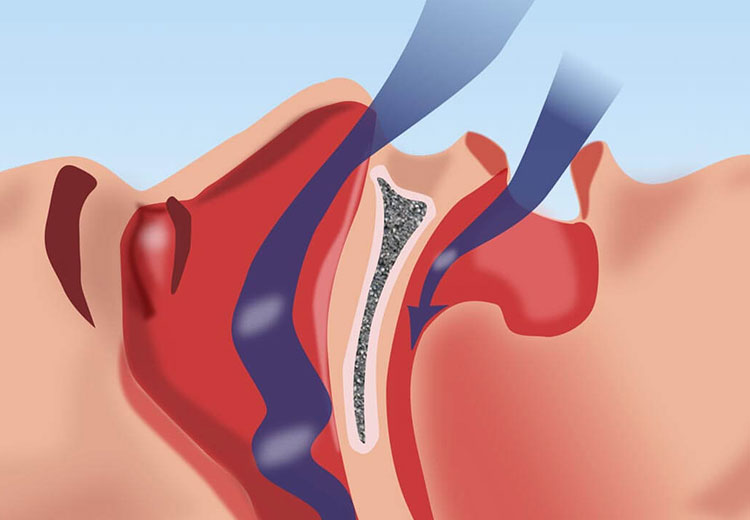
The Pillar Procedure is the procedure of placing three small implants in the soft palate to reduce the vibration of the soft palate, which is one of the anatomical elements of sleep apnea and snoring, which is effective in the sound of snoring, and the looseness that causes it to block the airway (Figure 2). When these implants are placed, they provide structural support to the soft palate. Over time, the fusion of the body’s natural tissue with these implants improves the structural integrity and stiffness of the soft palate.
Pillar implants are designed in such a way that they are not visible through the mouth and are not felt by swallowing or speaking, or do not interfere with swallowing or speaking. Implants can also be placed under office conditions with local anesthesia, and most patients can return to their normal diet and activity on the day of the procedure. This treatment method is preferred in patients who have simple snoring or mild sleep apnea detected as a result of sleep analysis and who do not have advanced deformity of the soft palate detected on physical examination.
The Pillar procedure can also be performed in combination with other surgeries for snoring and apnea.
Better results are obtained from this procedure in patients with a body mass index (Body Mass Index) below 25, such as Radiofrequency.
- Shortening of the small tongue (Uvulectomy):
The task of the uvula is to direct the food mass towards the upper part of the esophagus during swallowing, to prevent food from escaping into the nose and to facilitate the passage of the mucus stream from the nose into the esophagus.
Excessive snoring can lead to prolongation and thickening of the uvula by edema over time. In a very small part of patients, the cause of snoring and sleep apnea is a long and/or thick uvula alone. Therefore, uvulectomy is performed only in highly selected cases. The complication of uvulectomy is bleeding, although it is not common.
- Laser uvulopalatoplasty:
it is a technique that started to be used frequently with the introduction of LAUP (Laser Assisted Uvulo-Palatoplasty) in the early 1990s and can also be applied in office conditions. There are different opinions that recommend its use only in cases of simple snoring or in cases of mild to moderate sleep apnea.
The most important problem of laser LAUP is the severe pain that occurs after the procedure. This disadvantage has led to the abandonment of the technique to a large extent in recent years.
- Uvulopalatopharyngoplasty (UPPP):
It is the most commonly used surgical technique in patients with sleep apnea syndrome. Basically, the small tongue (uvula) is based on the principle of reducing the volume formed by the soft palate and tonsils (tonsils) (Figure 3). It is stated that it is successful in 85% of simple snoring patients and 25-75% of patients with sleep apnea syndrome.
After UPPP surgeries, temporary food escape into the nose (velopharyngeal insufficiency), bleeding, infection, nasal discharge complaints, swallowing difficulties, taste impairment and numbness of the tongue may occur. Caution should be exercised in the anesthesia of patients who are extremely overweight. The most common problem that patients complain about frequently is postoperative pain. Although it gradually decreases after surgery, significant pain complaints are often observed, especially in the first 5-7 days.
Dry mouth, a feeling of tension and nasal discharge, which can be a cause of long-term complaints, are caused by the inability of the uvula to perform its task.
B. OPERATIONS FOR THE ROOT OF THE TONGUE
After the soft palate region, the region most often responsible for snoring and sleep apnea syndrome is the behind-the-tongue region. For this reason, it may be necessary to perform intervention in both regions in many patients.
Especially if patients who are overweight and have a high body mass index (BMI) lose weight by 10% of their body weight, there is a high probability of a decrease in their complaints caused by the tongue root region. For this reason, if BMI is high in patients with problems detected in the root of the tongue in isolation, weight loss techniques should definitely be tried before surgery is planned. In case of moderate or severe apnea in patients with significant soft palate pathology, surgery for the nose and palate can be performed first. CPAP should be used in both groups if necessary during the weight loss study period.